Coccydynia Tailbone Pain Treatment with Craniosacral Therapy and Alternative Medicine in New York City
What Causes It?”
How Can It Impact Your Life?”
The Connection with the Central Nervous System”
Myofascial Trigger Point Therapy Treatment”
Craniosacral Therapy Treatment”
What is Coccydynia or Tailbone Pain
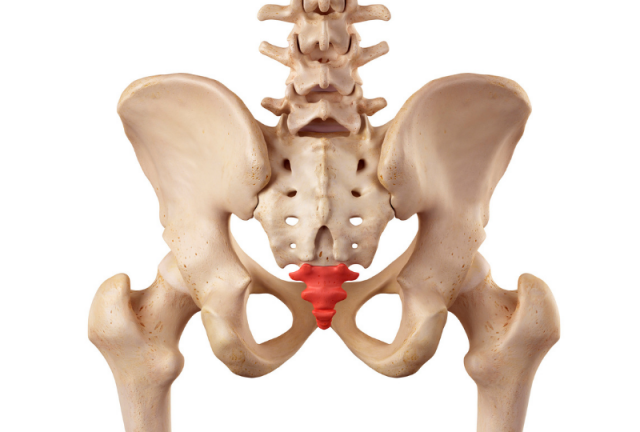
Coccydynia, also known as tailbone pain, is pain felt in or around the coccyx (tailbone) — the small, triangular bone at the bottom of the spine. The pain can be dull and achy or sharp and intense, making it difficult to do everyday activities. That’s because the coccyx provides stability when seated position, along with flexibility for the pelvis and hip bones with movement.
The main symptom of coccydynia is pain and tenderness at the base of your spine, specifically in the tailbone area between the buttocks that can sharply strike suddenly, vary in intensity and be constant or intermittent. The pain may worsen when sitting down, standing up, leaning back while sitting, or during bowel movements or sexual intercourse. In addition to pain, some people with coccydynia may also experience:
- Swelling or bruising around the tailbone
- Muscle spasms in the buttocks or pelvic floor
- Difficulty sitting & sleeping
- Severe headaches
- Constipation
- Lower back pain at the lowest part of the spine, may radiate to the hips, thighs, or rectum.
Pain that persists for more than three months is considered chronic and can affect all aspects of a person’s life. Fortunately research has shown 90% of those suffering with coccydynia can be relieved with non-surgical methods. If you have ongoing Coccydynia or tailbone pain and want relief, the final section of this information outlines the holistic treatments I offer to end your tailbone pain and comfortably resume your everyday activities.
What Causes Coccydynia or Tailbone Pain?
The tailbone (coccyx) is vulnerable to direct and often repeated traumas that can begin early in life and “snowball” with each repetitive microtrauma (sitting on hard surfaces over time). Additionally, a single trauma such as falling directly onto the tailbone or landing in a seated position can bruise, fracture, or dislocate the coccyx (tailbone). A single trauma or impact can slightly move the tailbone out of its normal alignment and restrict its mobility, causing constipation, lower back pain and more.
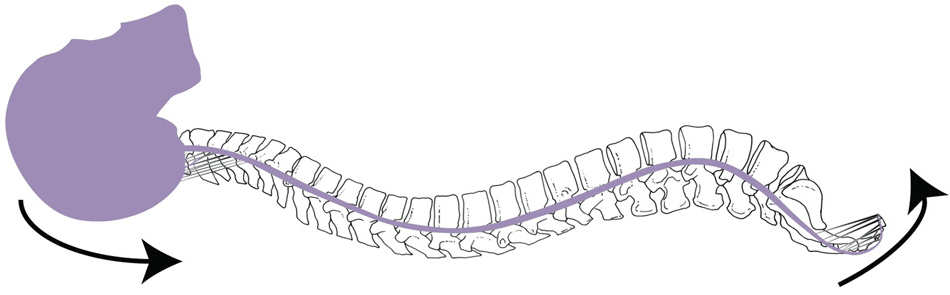
Single event trauma is not uncommon for women who injure their coccyx or tailbone during child delivery from the pressure of the baby’s head passing through the birth canal. In these situations, the coccyx may be pushed into an awkward angle enabling internal adhesions to form. Adhesions are bands of scar tissue which can lead to friction pulling on support ligaments, muscles and nerves in the region and can cause moderate to debilitating pain. A displaced coccyx (tailbone) can cause persistent or recurring headaches due to the pull (originated from adhesions) of the dura, a layer of protective membrane that surrounds the brain and spinal cord that stretches from tailbone to skull.
In general, activities that involve repetitive strain pressuring the tailbone or prolonged sitting on hard surfaces such as cycling or sitting in stadium seating, can strain the surrounding tissues and cause pain. Even something as simple as leaning back while sitting, the pain in your tailbone can increase due to additional stress and weight on the coccyx.
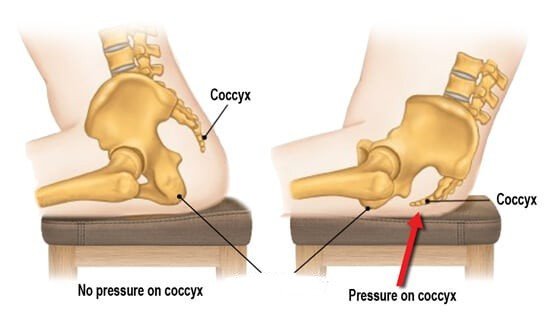
Also simply wear and tear or degenerative changes of the joints in the coccyx can lead to arthritis causing pain and inflammation. As the cartilage in the spine wears down, vertebrae may rub against each other, causing pain and any changes in the spine can also place excess pressure on the coccyx. Coccydynia can be exacerbated by excess weight (obesity), slouching while sitting, a lack of cushioning in the buttocks all can place additional pressure and strain on the coccyx or tailbone. In all of these situations, the coccyx may be stressed or pushed into an awkward angle disturbing support ligaments and nerves and causing moderate to debilitating tailbone pain.
How Coccydynia or Tailbone Pain Can Impact Your Life
Since the primary symptom of coccydynia is pain that worsens when sitting, it can definitely impact your ability to comfortably drive. The twisting and bending motions required to enter and exit a car can exacerbate tailbone pain, making it challenging to get behind the wheel or leave the vehicle. Furthermore, the movements involved in braking and accelerating can put pressure on the tailbone, triggering pain and making it harder to control the vehicle smoothly. Don’t attempt long drives without taking frequent breaks to stand up, stretch, and walk around. A coccyx cushion or wedge-shaped pillow can help relieve pressure on the tailbone while sitting.
Coccydynia can cause you to slouch or adopt other compensatory postures to relieve pressure on the tailbone. These postural changes can negatively affect your balance and coordination, making walking less efficient. Since the tailbone is involved in movements like walking, when inflamed or injured due to Coccydynia, walking can become uncomfortable. The muscles surrounding the tailbone, including the pelvic floor muscles, may become tense or imbalanced prompting restricted movement and or pain while walking. In some cases people avoid pain by altering their walking pattern, adopting an uneven gait or limp, which over time can cause strain or pain in other parts of the body producing a whole additional set of physical ailments.
Coccydynia can also make it difficult to find a comfortable sleeping position and can lead to frequent awakenings throughout the night. The pain can be persistent pain and then the anticipation of pain can also lead to anxiety, further delaying the ability to sleep. Even if you manage to fall asleep, the pain may wake you up during the night leaving you feeling unrested and tired the next day. The lack of sleep can worsen the pain and inflammation associated with coccydynia, creating a vicious cycle of pain, sleep deprivation, and increased pain and so forth.
Coccydynia or Tailbone Pain & The Central Nervous System
Coccydynia itself technically isn’t a nerve pain, but it triggers numerous types of nerve pain because the coccyx has a vast network of nerves traversing nearby, and injury or inflammation can directly irritate these nerves, leading to localized pain in the tailbone area.
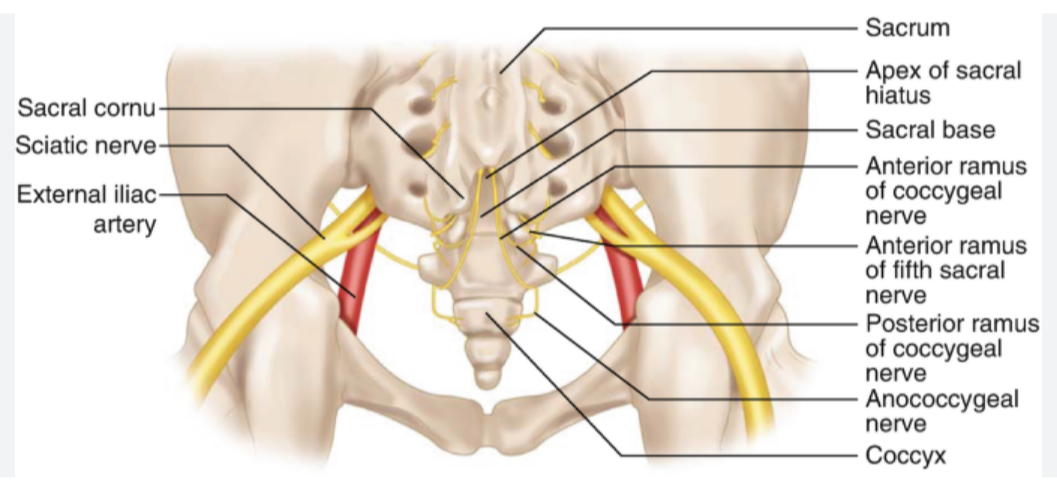
Coccydynia or Tailbone pain is driven by the many nerves that transmit pain signals to the spinal cord and brain through the central nervous system. In some cases, chronic coccydynia can lead to central sensitization, a phenomenon where the central nervous system becomes more sensitive to pain signals, leading to increased pain perception and a lower pain threshold. This can make the pain feel more intense and widespread.
Also, pain from the coccyx can transfer to other areas, such as the buttocks, hips, lower back, or even the legs. This is known as referred pain and stems from how nerves from different areas converge in the spinal cord. Coccydynia can sometimes cause nerve damage or dysfunction, leading to neuropathic pain, which is a type of pain that originates from the nervous system itself. This pain is often described as burning, tingling, or electric-like sensations.
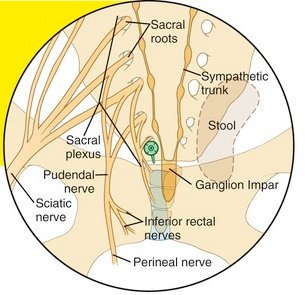
Sometimes the pudendal nerve, which runs near the coccyx, can be affected by Coccydynia. This can lead to pudendal neuralgia, characterized by pain, burning, or numbness in the genitals, perineum, or rectum. Also nearby is the ganglion impar, a collection of nerves that if irritated or compressed can radiate pain in the tailbone area, genitals, or rectum.
The experience of chronic coccydynia can also affect the central nervous system and lead to changes in mood, sleep, and stress levels. These changes can, in turn, worsen pain perception and make it more difficult to manage. Understanding the connection between coccydynia and the central nervous system is key for appreciating the unique aspects of my treatment program to resolve tailbone pain. The therapy I offer targets both the peripheral nerves in the coccyx region or in other words, “the central mechanisms of pain processing”.
Treating Coccydynia or Tailbone Pain with Myofascial Trigger Point Therapy
Treating the tailbone starts with ensuring the nearby region including the muscles in the buttocks, hips, and lower back, are free of tight muscular trigger points or fascia restrictions. Fascia is the network of collagen and elastin connective tissue permeating the entire body, including just beneath the skin and surrounding all muscles and organs. For example, the buttocks or gluteus maximus, which extends the thigh, has attachments at the coccyx and sacrum.
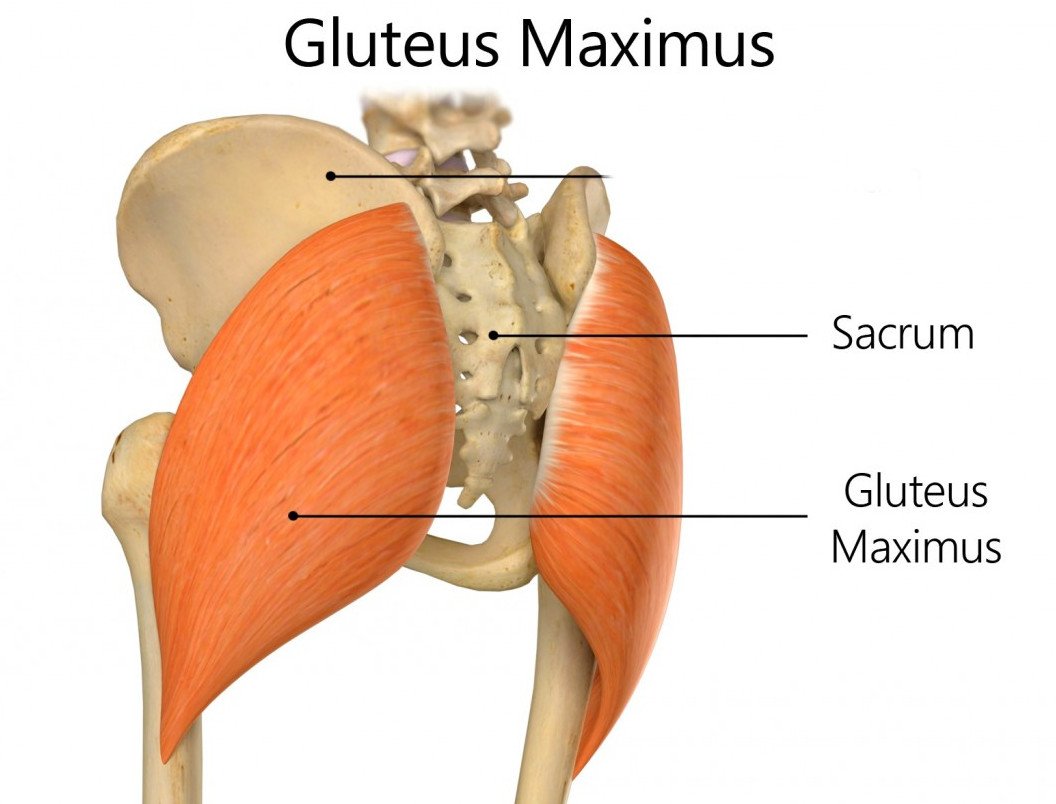
Identifying and freeing fascia adhesions in this region that developed in response to falls or repetitive microtraumas, such as poor seating or posture, helps correct and restrict mobility or imbalances of the sacrum, pelvic bones and joints and the coccyx. Since pain emitting from the tailbone or coccyx can originate from or be exacerbated by issues in nearby regions, it is important to inspect, and if need be treat, areas of the hip or the low back for fascia adhesions and any consequent spasm, tightness or tensions.
Myofascial trigger point therapy effectively eliminates fascia adhesions and those points in the muscles (trigger points) that can refer pain to other areas of the body. In the case of coccydynia (tailbone pain), trigger points can develop in the muscles of the pelvic floor, gluteal muscles, and lower back muscles. These trigger points can cause pain in the tailbone itself, as well as referred pain to the hips, lower back, and even down the legs. By applying pressure to these trigger points, Myofascial therapy can:
- Release tension and tightness in the muscles, which can reduce pain in both the trigger point and the referred pain areas.
- Restore normal muscle function and improve strength.
- Improve muscle flexibility and range of motion.
Myofascial treatment slowly relaxes all tissues and the molecular-chemical bonds binding collagen fibers and creating adhesions seemingly detach or dissolve away. This then allows the bones and joints to return to their earlier and proper symmetry and improved mobility that was in place prior to the coccydynia. Long-term pain resolution requires decreasing the underlying adhesions that attach to the coccyx, pulling it out of its normal alignment and causing pain or dysfunction. Myofascial trigger point therapy is often used in conjunction with other therapies for coccydynia, and I often apply craniosacral therapy, a gentle, hands-on therapy that focuses on the bones of the skull, spine, and sacrum.
Treating Coccydynia or Tailbone Pain with Craniosacral Therapy
“The nerves of the coccyx include somatic nerve fibers and the ganglion impar, which is the terminal end of the sympathetic nervous system.” Source, National Library of Medicine Research
Craniosacral therapy is founded on the concept that the body possesses an innate ability to heal itself; however injuries can lead to restrictions in the craniosacral system, affecting the function of the central nervous system and potentially causing various health issues. Craniosacral therapy aims to improve the sympathetic nervous system by revitalizing the craniosacral system, which includes the membranes and cerebrospinal fluid that surround and protect the brain and spinal cord. Thus targeted delicate manual manipulation of the rhythmic motion of cerebrospinal fluid that surrounds and protects the brain and spinal cord, any blockages or restrictions in this craniosacral system can be removed enabling the optimization of the functioning of the central nervous system.
Craniosacral therapy aims to reduce the fight-or-flight response, promote relaxation, balance the autonomic nervous system, and improve the terminal end of the sympathetic nervous system, the coccyx. More precisely and as noted earlier, the pudendal nerve which runs near the coccyx, can sometimes be affected by coccydynia leading to pain, numbness, or dysfunction in the region. Craniosacral therapy treats pudendal nerve irritation indirectly through releasing any tightness, restrictions or inflammation of the pudendal nerve’s surrounding fascia (connective tissue). Craniosacral therapy can also gently manipulate the sacrum and other pelvic bones to improve any misalignment and reduce pressure on the pudendal nerve.
Much the same applies for the ganglion impar, a nerve bundle located in the pelvic region, surrounded by fascia, as it is responsible for transmitting pain signals from the coccyx (tailbone). Craniosacral therapy can gently release fascial restrictions around the coccyx and pelvic floor, potentially reducing pressure on the ganglion impar.
Since in some cases, chronic coccydynia can lead to central sensitization, a phenomenon where the central nervous system becomes more sensitive to pain signals and is associated with neuroinflammation, a chronic inflammatory process in the nervous system. Craniosacral therapy is a therapeutic response to central sensitization and can help to activate the parasympathetic nervous system, promoting relaxation and reducing pain perception.
The Following Services are Offered by Dr. Kaminsky, Craniosacral Therapy which facilitates the body’s innate regulatory and healing ability by stimulating, through the focused touch of the therapist, flow of Cerebro-Spinal Fluid throughout the body.
LINK: Most Frequently Asked Questions About Craniosacral Therapy – Craniosacral Therapy NY
Myofascial Release: Decreases pain and improves movement by activating muscle and underlying fascia to uptake more vital fluid available in the body for optimal structural and functional integrity.
LINK: Myofascial Release Therapy NYC (craniosacraltherapyny.com)
Somato Emotional Release (SER) Helps the body release trapped, stuck negative experiences / emotions resulting in restructuring of the nervous system and a reversal of symptoms and various ailments of the mind-body.
Link: Somato Emotional Release Therapy in New York City (craniosacraltherapyny.com)
Vagus Nerve Toning: Recalibration of the nerve often referred to as the Rest and Digest part of the nervous system. Best done with specialized vibrational sound healing tunning forks of 128 hz frequency.
LINK: Vagus Nerve Treatment with Chiropractic Care in New York City (craniosacraltherapyny.com)